With the help of orthopedics and trauma surgery, congenital hip deformities can be corrected and femoral neck fractures can be treated. Even with severe damage to the hip joint, for example due to wear and tear due to osteoarthritis, patients can move independently thanks to modern artificial joints and lead an active life.
Hip joint surgery is done when conservative therapy is ineffective or in case of emergency. Modern medicine has a wide range of techniques for joint treatment, and high quality rehabilitation methods can help you to return to a life of full value after an intervention.
Surgical treatment of the hip joint is required when bone tissue is severely damaged by progressive diseases of the musculoskeletal system. In this case, joint replacement is necessary.
Before the intervention, additional examination is carried out to study the manifestations of pathology and reduce risk factors. For various types of hip joint surgery, contraindications can be different because they depend not only on general recommendations, but also on systemic factors, such as age, concomitant diseases, blood disorders and the nature of the intervention (primary or secondary).
But in most cases, surgery is not performed if a patient has one or more of the following diseases:
- Severe chronic cardiovascular diseases
- Cardiac or respiratory failure that can cause problems with anesthesia and other complications
- Open form of tuberculosis
- Purulent inflammation of the hip joint
- Progressive chronic infection in the body
- Neurological or mental disorders
- Metastatic cancer
Arthrotomy and Hip Joint Resection
Hip arthrotomy is any surgery involving hip joint opening and providing intraarticular access. It is used for:
- removing purulent exudates, free bodies and foreign bodies in the joints;
- correcting old or congenital joint dislocations;
- resection hip joint tumors or infectious foci;
- arthroplasty in case of ankylosis.
As already said, resection of the hip joints mostly is an atypical operation, often of a more extended type as that for closed coxitis. It should be performed with the utmost accuracy, adhering to the general rules reassigned in protocols.
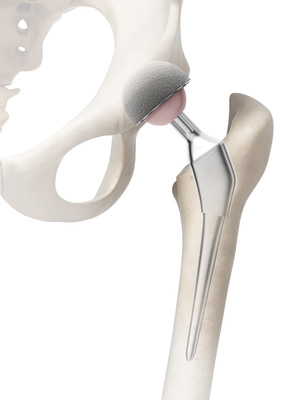
Osteosynthesis
Conservative treatment of patients with severe hip injuries is not very promising: it leads to complete immobilization for a long time, difficult rehabilitation, whilst there is no any guarantee of success. It is especially related to the older people with weakened calcium metabolism and osteoporosis. So, non-surgical options are used for them only when surgery is contraindicated.
Young people also hardly can like the complete immobilization. Therefore, always when possible, osteosynthesis of the femoral neck is considered in the first place.
Indications for osteosynthesis are following:
- Basal fractures of the femoral neck in patients with active lifestyle
- Transcervical damage in bone integrity (fractures) in people under 60
- Punctured fractures
- Subcapital neck of femur fractures (NOF)
- There are contraindications to joint replacement
There is a variety of concepts of metal osteosynthesis for the neck of the femur fractures. Many different factors influence the process of selection a particular method of reposition and osteosynthesis. Closed reduction of bone fragments with use of screw fixation is one of the well-proven techniques.
Closed reduction has a number of great advantages:
- It is a minimally invasive technique. As a rule, no more than three (sometimes two) screws are required.
- It does not take much time, which is important for combined injuries.
- It is just perfect for fixing fragments in case of intraarticular fractures.
- It provides a high level of reduction and immobilization of bone pieces.
- Titanium alloy does not cause rejection and complications in patients after surgery.
- The screws are easily removed after the consolidation of hip fracture.
The fixation, which is achieved by different ways, can be:
- Relatively stable: slight micro movements between bone fragments are possible, but they do not cause pain and, furthermore, contribute to coalescence of fragments by forming a periosteal callus.
- Absolutely stable: there are no any movements between bone fragments in the damaged area.
The core feature of the method is a special mode of screw fixation. Screws are screwed into the bone at the twisted thigh bones area, pass inside the femur neck in parallel to its surface and end in the central part of the femur head.
The start and end points were chosen not by chance, since the density of bone tissue is maximal in these areas, which ensures a high stability of the fixation of the bone fragments – what is needed for a better bone healing.
On practice, the best effect of osteosynthesis with screws is achieved for locomotor fractures, provided that displacements of the bone pieces are relatively small.
Ultrasonic osteosynthesis also deserves to be mentioned: with this method, connecting fractured fragments, filling the hip joint cavity and creating bone conglomerates in order to restore bone integrity are done by means of ultrasonic welding.
Osteotomy
Joint surgery involving an excision or fracture of the bone with medical instruments to eliminate deformation is called hip osteotomy.
Osteotomy is performed on the hip joint when there are violations of the functions of the musculoskeletal system or deformations of the bones. For the hip joint, this surgery is performed in the case when the femoral head and the hip socket are not aligned properly.
Frequent causes of such pathology are cerebral palsy (CP), joint dysplasia, osteoarthritis, and Legg-Calve-Perthes disease.
During this operation, a surgeon corrects the shape of the femur neck and, then, rotates the acetabulum for a better alignment. Healthy cartilage is replaced and, due to this, the femur head has a good covering that does not allow it to move.
The surgery is performed under general anesthesia; its duration is about 2 hours. After the surgeon corrected the bone deformation, a plaster cast is applied to be worn for about 7-8 weeks. After it is removed, the patient, at first, moves with crutches in order not to overload the joint, but after some time he or she can return to normal activities.
Arthroscopy
Hip arthroscopy is a surgical procedure that is performed with a special device called an arthroscope. It is equipped with ultra-precise optics and light and used for diagnosing and treatment of diseases of the hip joint. The main advantage of arthroscopy is low trauma, since they are carried out through a small incision and minimally damage soft tissues.
Arthoscopy of the hip joint is indicated when the diagnosis requires extensive examinations and numerous studies. A regular pain in the groin or in the pelvic area can be an indication for arthroscopy. During this procedure, it is possible to remove free bodies and to eliminate damage cartilage from the hip joint.
During arthroscopy, the surgeon examines the space between the hollow of the thigh, the femur head and other areas of the hip. All manipulations are performed under general or local anesthesia. The operation is carried out with a stretched leg, which allows doctors to ease access to the damaged area.
The following diagnoses may be a reason for surgery:
- joint rupture;
- free bodies, namely cartilage fragments, in the joint;
- snapping of the hip joint;
- arthritis on early stage;
- cartilage damage of different origin.
The undisputed advantage of arthroscopy of the hip joint is quick recovery. It is much easier and with lesser pain than with open hip surgery. Starting from the very first day after surgery, patients have to do special exercises to restore joint mobility. The patients who have limp are advised to use crutches or walkers for one and a half to two months after the surgery. Later, patients can try to start light physical activities, such as cycling or swimming. Usually, the recovery takes from three to four months; however, in more complex cases, a longer recovery may be required.
Atrodesis
Arthrodesis is a surgical technique intended to return or improve support ability of the joints by fixing them in an immobile state. There are some cases when, without this procedure, you can get limited ability to move, or even complete disability. This treatment has some specific features. Please note, that arthrodesis is not indicated to all patients, even though their symptoms are similar.
Hip arthrodesis is one of the possible surgical interventions to treat deforming osteoarthritis. This type of surgery is aimed to stabilize the joint by immobilization. Trauma surgeons use this a method when it is necessary to reduce or eliminate the symptoms of pain syndrome, but, for some reason, arthroplasty and hip replacement are contraindicated.
There are four methods of arthrodesis mostly used:
- intraarticular;
- extraarticular;
- combined;
- compression (open or closed).
This procedure may be required at the following joint diseases and conditions:
- Dangling joint: complete or partial misalignment of the joint, causing limited or complete atrophy of intraarticular mobility (flaccid paralysis syndrome, ligament integrity damage, consequences of gunshot wound, genu recurvatum, etc.).
- Deforming arthritis: pathological deformity or tuberculosis of bones and osseous joints, acute purulent or traumatic arthritis.
- Complicated osteoarthrosis: degenerative dystrophic diseases of the joints, characterized by damage to the cartilaginous tissue of the articular surfaces.
- Consequences of poliomyelitis (cerebral palsy).
- Improperly fused / fusing fractures.
- Impossibility of plastic surgery on problematic joints using a partial / total endoprosthesis or plates;
- Other causes that lead to reducing of active movements in the joint and increasing of passive movements.
During the surgery, all functionally altered tissues are removed and cartilage of the femur head and acetabulum is excised, as well as the spongy layer of the bone. The articular surfaces are joined in such a way to provide later their reliable fusion. In case when the femur head and the main part of the femur are not viable, they have to be resected. After the surgery, a plaster cast is applied that are removed after not less than three months.
After the plaster cast is removed, an X-Ray scan is done for a check-up. With satisfactory fusion, another plaster bandage is applied for 3-4 months more. Six months after the surgery, the patient can walk.
Rehabilitation
The treatment you will receive at the Medical Center depends on the implant type and doctor prescriptions.
The first few days after surgery are the most important. Your body is exhausted, and you have not yet fully recovered from anesthesia, but already in the first hours after you have come to consciousness, try to remember about the operated leg more often to be mindful about its position. As a rule, immediately after the operation, the operated leg is placed in a slightly flexed position. There will be a special bolster between your knees placed so to ensure their moderate spreading. The active regime in bed is allowed already in the first day after the surgery.
The first time you need to change bandaging is the next day after the surgery, and later on it will be done when needed, but at least once every 2-3 days until complete healing. 12-14 days after the operation, the stitches are removed. Sometimes, the wound is sutured with absorbable threads andyou don’t need to remove them.
In the first 2 days after the operation, a light diet consisting of porridge on water, jellies and fermented milk products is prescribed. Food, boiled or steamed, is given in semi-liquid or puree form, with the limitation of refined sugars and salt. Products promoting bloating and fermentation processes should be excludedfrom the ration. Next, one of standard diet plans is prescribed, considering the concomitant diseases.
Any operation has a risk of blood clots in the leg veins. You will be prevented from this complication by elastic bandaging of the lower extremities, and the prescription of anti-clotting medications.
Please remember that:
- In the first days after surgery,you should sleep only on your back.
- When turning in bed on a healthy side, you have to use a bolster between the legs, holding it with your knee slightly bent and ankle joints.
- In the first days, you should reduce a range of movements in the operated joint, and, especially, avoid bending in the knee and hip joints for more than 90 degrees, sharp turns of the leg, and rotation in the hip joint.
Recommended loads on the operated leg:
In case of cemented fixation:
- Partial load: from the first days after surgery
- Full load: by the end of the 1st month
In case of cementless but strong fixation:
- Partial load (15% of body weight):after 7-10 days
- Partial load (50% of body weight): by the end of the 3rd week
- Full load: by the end of the 2nd month
In severely weakened patients (suffering from acute cerebrovascular disease, severe somatic pathologies, cancer patients, and in people older than 90 years):
Full load: immediately after surgery
In patients with acute pain:
Immediate load limitation (in any period of time)
Physical Therapy
Try to devote all your free time to physical therapy. At first it will be accompanied by a moderate pain, but every day it will become easier.
The main goal of physical therapy is to improve the blood circulation to the operated hip, to prevent thrombosis, reduce edema, and speedup wound healing.
Another important task of physical therapy is strengthening the muscles of the operated limb, restoration of the normal range of movements and ability of the joint to support the entire body weight. Remember that anartificial joint is a bearing with an ideal slipping and minimal friction force. And that is why it is better to exercise actively in order to strengthen the muscles surrounding the joint rather than passive rocking and stretching.
In the first 2-3 weeks after the surgery, you should exercise lying in bed. All exercises must be performed slowly, evenly, and avoiding sudden movements and excessive muscle tension. To breathe correctly while exercising is also very important: breathe in when you strain muscles and breathe out when you relax.
1st exercise is to the gastrocnemius muscles. Gently push your feet up and down. Do this with both feet for several minutes up to 5-6 times in an hour. You can do this exercise immediately after awakening from anesthesia. Clench and unclench your toes.
Starting from the second day after the operation, continue with the following exercises:
2nd exercise is for the hip muscles. Keep your legs straight. Strengthen your knee pressing the knee pits to the bed and hold this tension for 5-7 seconds, then slowly relax.
Buttocks muscle strengthening:
- Toning up the back part of the thigh and lower leg: press the heels to the bed for 5-7 seconds, then, slowly relax
- Moving the leg aside along the bed surface and bringing it back
3rd exercise: Cautiously slide your foot on the surface of the bed toward your buttocks bending the leg in the hip and knee joints. Then slowly slide it back. When doing this exercise, at the beginning you can use with a diaper or elastic tourniquet, by placing it under the knee. Remember that the angle of bending at the hip and knee joints should not exceed 90 degrees!
4th exercise: Put a small pillow under your knee (not more than 10-12 centimeters) and try to strain the muscles of the thigh slowly and straighten the leg at the knee joint. Hold the straightened leg for 5-6 seconds, and then slowly lower it to its original position.
Do all the above exercises through out the day, for several minutes every hour (5-6 repetitions each).
From the second day you can sit down on the edge of the bed, leaning on your elbows, or holding on to the handrails with your feet lowered to the floor. First, you should gradually move the healthy leg, and, then, drag the operated one over it. Your legs should be moderately apart; you can ensure this using a bolster. To move the operated leg, you can use a special elastic bandage. When you move the operated hip to the side, keep the body straight and do not let your leg roll outward.
Always remember to bandage your feet with elastic bandages before you sit down or get up, or wear special elastic stockings to prevent thrombosis of the veins of the lower extremities. To restore normal movement of the joint, from the second day you will start a physiotherapy course with the help ofmechano-therapy appliances, special devices that, according to a specially designed program, will bend and unbend your leg in the hip joint. However, although those simulators are effective, they will not replace your own efforts. You will need to practice and develop your muscles so that they are ready by the time when you are able to walk without help.
First Steps
The purpose of this rehabilitation period is to learn how to get out of bed, stand, sit and walk without help and safely.
As a rule, you are allowed to get up on your own on the second day after surgery. The first time you should get up only under supervision of medical staff. You are still weak and someone must help and assist you. You may feel slightly dizzy, but try to rely on your own strength as much as possible. Remember, the earlier you get up, the earlier you start walking by yourself.
Get out of bed from the side of the healthy leg. Sit on the edge of the bed, keeping the operated leg straight and extended forward. Place both feet on the floor. Using crutches, step on the non-operated leg and try to stand up. Leaning on the healthy leg, move the crutches forward. Then, slightly bend the operated leg in all joints and move it too. Leaning on the crutches, transfer your weight to them and push forward the healthy leg. Repeat all movements in the same order.
In the first 7-10 days, you can only touch the floor with the foot of your operated leg. Then, slightly increase the load through your leg, trying to step on it with a force equal to the weight of your foot, or 20% of your body weight. You should regulate the time you walk taking into consideration how you feel andcondition of your leg, and without reducing exercise therapytime. If you exercise not enough or do it incorrectly, and, at the same time, walk too long, by the end of the day you will have swollenfeet. In this case, consult a doctor. Concomitant diseases also may contribute to swelling.
After you have learned to stand steady and walk without help, you may start exercising whilst standing, with your hands on a support.
1st exercise: Moving a straightened leg forward
Stand on the healthy leg with your hand resting on the back of a bed or chair. Slowly move the operated leg forward by 20-30 cm. Make sure that the thigh, knee and foot directed forward. Keeping the same pose, slowly bring your foot back to its original position.
2nd exercise: Moving the legaside
Standing on the healthy leg with your hand resting on the back of a bed, slowly move the operated leg to the side for 20-30 cm. Make sure that the thigh, knee and foot directed forward. Keeping the same pose, slowly bring your foot back to its original position.
3rd exercise: Moving your foot back
Standing on a healthy leg with your hand placed on your loin, slowly move the operated leg back. Make sure that the waist does not bend. Slowly return to the original position.
4th exercise: Raising the knees
Slowly bend the operated leg in the hip and knee joints by an angle not exceeding 90 degrees and raise the foot to a height of 20-30 cm above the floor. Try to hold the raised leg for a few seconds, then, slowly lower the foot and put it on the floor.
The above exercises are recommended to do up to 10 times a day for 5-15 repetitions.
Learning to Climb and Descend Stairs
So, you walk on crutches quite confidently in the ward and hospital corridor. But in everyday life,it is not enough. You need also walk up and down the stairs. If you have only one joint replaced, you start climbing should be from the un-operated leg. Leaning on crutches, transfer the leg to the next step. Move the crutches over it and transfer the weight of the body to the un-operated leg that is now standing a step higher. Then lift the operated leg and put it on the same step. Crutches are moved last or simultaneously with the operated leg. When descending, you should first move the crutches, then, the operated leg, and, finally, the un-operated one.
More exercises to restore motor functions
1. Lower leg muscles
Take a position lying on your backwith arms and legs spread out. Tighten the abdominal muscles. Pull the toes up and press the heels to the floor. For a few seconds, keep the tension in the lower leg muscles and, then, relax.
2. Extensor muscles
Take a comfortable position lying on your back, with your arms and legs spread out. Tighten the abdominal muscles. Press the knee pit to the pillow under your knees, and pull the toes up. For a few seconds, keep the tension and, then, relax.
3. Muscles of the buttocks
Take a position lying on your back with arms and legs straightened. Tighten the abdominal muscles. Pull the toes up. Do not bend your knees. For a few seconds, strain the buttock muscles, and, then, relax.
4. Bendingat the hip
Place something you can slide on it (for example, a towel) under the foot of the operated leg. Raise the operated limb bending it in the knee, while simultaneously pressing the heel to the towel and pulling it toward the buttocks. When you do it, the toes are moved up. Hold the limb in that position for a while, and, then, return the foot to its original position.
5. Moving the legaside
Take the position lying on your back, stretching your legs. Place something you can slide on it (for example, a towel) under the foot of the operated leg. The toes should point to the ceiling. Slightly move your leg to the side, then, slowly return it to its original position. During the exercises, the knees should not touch each other.
6. Bendingat the hip joint
Take the position lying on the back, so that the operated leg is slightly bent. After this, raise the limb bending the knee at 90°, and keep this position for some time. Slowly return the bent leg to its original position. During the exercise, the healthy leg should be straight and remain on the floor. The toes are pointed upwards.
7. Moving your leg to the side
Take a comfortable lying position on the healthy side. Place a pillow between your legs. Bend the healthy leg and place a bent arm under the head. Put your head on your arm. Raise the operated leg, hold on for some time, and then return to its original position. When lifting your legs, keep them straight. Do not straighten your toes and keep your feet parallel to the floor.
8. Moving a bent leg to the side
Take a comfortable position lying on a healthy side. Place a pillow between your legs. Bend both legs in the knees. Slowly raise the operated one up, hold on for some time, and, then, return it to its original position. Do not straighten your toes, while the knee should be pointed forward.
9. Moving your leg to the side
Place a durable object of a small heighton the floor, and stand on it with a healthy foot. It is necessary that you stand slightly up so that the operated leg does not touch the floor. To keep balance, your hand is resting onthe chair back. Move the operated leg aside, and then return it back. The leg should be straight, but the toesare not stretched.
10. Unbending in the hip joint
Stand in front of the chair with your hands on its back. Move the weight of the body to a healthy limb. Slowly move the operated leg back without bending, and then return it to its original position. When doing the exercise, the upper body should be straightened.
11. Bending the knee
Stand in front of the chair with your hands on its back. Slowly bend the leg at the knee and lift it. Keep such a tense position for some time, and, then slowly lower your leg. The knee should be directed forward, and the foot should be parallel to the floor.
12. Straightening at the hip joint
Take the position lying on the abdomen, while the legs are straightened and the arms are stretched above the head. Bend the operated leg in the knee. Raise the hip upward with the knee bent. Keep this position for some time. Slowly lower your foot to the floor, still keeping the knee bent. Finally, straighten the leg, returning to its original position. Relax for a moment and, then, repeat the exercise.
13. Extension in the knee and hip joints
Ask a doctor if you can do this exercise. Take a position lying on your stomach with a pillow under it to prevent the waist from excessive bending. Stretch your arms above your head. Place the roller under the feet, so that the toes are pointing towards the floor. Raise the knee above the floor with the back of the knee toward to the ceiling. Raise the straightened leg until you feel the tension in the muscles of the thigh. Hold the limb in this position for a while, then relax and return the leg to its original position on the roller.
What advantages and risks does an artificial hip joint have?
Improvements after joint replacement
The artificial hip replacement is one of the most successful surgical procedures in modern medicine. Prerequisites for a good result are the correct selection of the procedure, a successful surgical procedure, the close cooperation of all participants in the follow-up treatment and appropriate behavior of the patient. If these prerequisites are met, a significant improvement in pain or even pain relief can often be an effective improvement various functions as well as a restoration of the overall quality of life can be achieved. These include after completed recovery time and the
Ability to improve locomotion: usually longer walking and hiking or cycling and use of cars and public transport again much better possible than before the operation.
Tightening and body-care relief: With improved mobility it is often possible, e.g. Wear socks and shoes or do the foot care (cutting the toenails) yourself. However, this can take a long time, because in the first 6 weeks after surgery, the flexion of the hip joint is limited. Depending on the soft tissue tension, longer-term restrictions may also remain with pedicure.
Participation in meaningful sports activities: Many patients expect their joint replacement surgery to improve their participation in sports activities. In one of the following chapters (My Life with the Articular Joint - What To Look For?) Suitable and less suitable sports are described in detail. Basically, with often existing improvement of pain and dysfunction after the operation also sports activities can be resumed or continued. However, other influencing factors on sports ability as a whole must be taken into account realistically: these include, in particular, the age of the child, the experience previously accumulated in one sport and, above all, the duration of a sports ability that might not have existed before the operation. The longer no sport has been practiced, the more difficult the return can be. Nevertheless, from a medical point of view, participation in sport is almost always supported under the conditions to be observed.
Improvement in other areas: Depending on their particular problem situation, patients often have very different expectations of an improved outcome after joint replacement. These include, for example, the elimination of pain during sexual intercourse, a possible return to social activities or the improvement of their employment in the workplace, household and leisure as a whole. Often there are effective improvements in these areas. However, it should always be attempted to discuss the individual wishes and expectations in a joint doctor's discussion before the intervention, so that the surgeon can respond to the individual situation and advice on realistic goals is possible.
Risks and complications of hip replacement
As the intake of medicines is associated with possible side effects, there are also special risks in artificial joint replacement. The following lists the main risks that a patient should be informed about. Where possible, an indication is given as to which statistical frequency the occurrence of a complication must be expected. Fortunately, although fortunately, this damage is relatively rare, it is never possible in an individual case to accurately estimate the personal risk situation. Therefore, it is of particular importance to express significant concerns and concerns in the doctor's talk.

































 Loading ...
Loading ...


